Symptoms
Primary and secondary forms of bedwetting
Every child develops at a different rate - while some children can walk at 10 months, others take their first steps at 18 months. The journey to getting toilet trained is no different. Depending on when a child achieves full bladder control, it can happen quickly or take longer.
But at what age should the bed start to stay dry at night? As a rule of thumb, if a child wets the bed at least 2 nights a month after the age of 5, this is called "bedwetting" (medically known as nocturnal enuresis).
It has two different forms:
- The primary form of bedwetting is when your child has never been able to stay dry for a prolonged period of time since birth.
- The secondary form is when your child starts to wet at night after a dry spell of at least 6 months. This often happens when there are changes in the environment, such as the birth of a sibling or the divorce of parents. On the other hand, recurrent bedwetting in children can also indicate a urinary tract infection.
Wetting at night and during the day
If a child wets himself/herself during the day, this is called incontinence. The primary and secondary forms of bedwetting often occur together.
As parents, you should know that you are not alone. If your child wets the bed (again) at night, you are one of many families affected. Statistics show that enuresis is the second most common disorder in children after allergies - but because hardly anyone talks about it, this fact is usually unknown.
How many children are affected by nocturnal enuresis and at what age? 1,2
| 4 years | 7 years | 10 years | 16 years |
| 25 – 35 percent | 10 – 15 percent | 5 – 7 percent | 1 – 3 percent |
Boys are more often affected than girls. If the symptoms are not treated, 1-3 percent of adolescents still wet themselves at night.
Trigger
How does bedwetting occur?
Important to know:
Ultimately, only your paediatrician or urologist can determine the causes in your specific case through questioning and examination.
Delayed development of bladder control
Most children gain control of their bladder function by the age of 5. This maturation process is delayed in children with bedwetting. The interaction between the bladder and the brain is not yet perfect. This minimal developmental delay goes away on its own in many children.
Insufficient bladder capacity
If the bladder capacity is smaller than normal for your child’s age, your child may not be able to store the urine produced during the night. Children with a very small Bladder also go to the toilet a lot during the day.
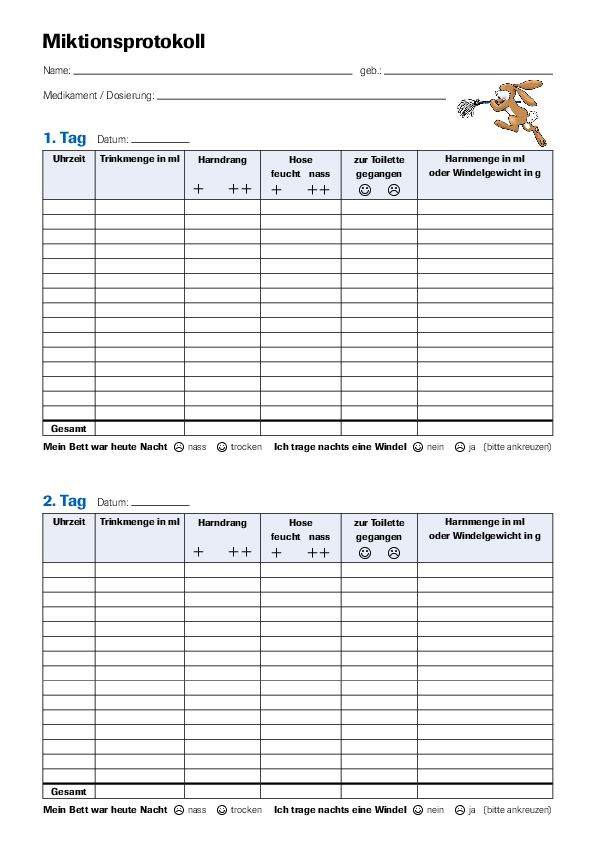
This is relatively easy to find out with the help of a micturition diary - in this pee diary, you record when and how often your child goes to the toilet during the day and how much urine he or she passes.
Download the micturition diary (pdf, 31KB)
Heredity
Numerous studies have shown that primary bedwetting is far more common in some families than in others. This fact allows conclusions to be drawn about the hereditary nature of the disorder.
If other people in your family have or have had nocturnal enuresis, your children are more likely to suffer from bedwetting too.
Antidiuretic hormone (ADH, vasopressin) deficiency
The antidiuretic hormone has a decisive impact on urine production. It is mainly released at night. It ensures that the kidneys secreteless urine and the bladder does not need to be emptied during sleep. It puts the body in night mode, so to speak.
This day-night rhythm of antidiuretic hormone production may not be fully developed in children suffering from primary bedwetting. As a result, the kidneys produce too much urine during sleepand the normal capacity of the bladder is exceeded.
Difficulty in waking up
Children who suffer from bedwetting are often not woken up by the stimulus of a full bladder during the night. They sleep so deeply that they don't wake up when they need to go to the toilet.
Drinking habits
Your child's drinking habits are very closely linked to enuresis. If your child drinks too little in general, his or her bladder is missing an important stimulus and may not be able to develop age-appropriately. If your child drinks majority of fluids during the second half of the day and especially in the evening, this can aid night-time wetting.
Does my child drink enough?
The German Nutrition Society (DGE) recommends that children between the ages of 4 and 10 drink just under 1 litre a day.3 Older children and adolescents should drink around 1.1 to 1.3 litres a day - more if they are into sporting activities or in summer temperatures.
Give your child mainly water or unsweetened tea. Avoid lemonade, ready-made iced teas or juices - they contain a lot of sugar.
Psychological problems
Changes in life circumstances also affect your child and can be a psychological cause of bedwetting in children. For example, the birth of a sibling, moving to a new neighbourhood, problems at nursery or school or parental separation sometimes play a role in secondary bedwetting, i.e., wetting after a dry spell of at least 6 months.
Don't put pressure on your child, but try to react with understanding. If the problem does not go away on its own, make an appointment to see your paediatrician.
Read on to find out how the doctor makes a diagnosis and how you can work together to find the right treatment.
Diagnosis
What can the doctor do about bedwetting?
Treatment
Treatment of bedwetting
Before treatment for bedwetting can begin, your consulting doctor will need to make a clear diagnosis or find out the exact cause. It is on this basis that he/she can decide which treatment is suitable for your child. There are various treatment options for both the primary and secondary forms of bedwetting.
![[Translate to English:] Mutter ist mit ihrem Kind wegen Bettnässen bei einer Ärztin.](/fileadmin/_processed_/1/8/csm_Mutter_mit_Kind_Bettn%C3%A4ssen__1__47557cfa8d.png)
Motivation and patience
Whichever treatment option you and your child decide on, the success of the therapy largely depends on your child's motivation.
At the beginning of the treatment, everything is still new and interesting and the initial successes are usually not long in coming. However, as time passes, other things attract the attention of the little patients. Then there is the possibility of relapse and the disappointment for the child and parents is great.
In this situation, it is your job to continuously motivate and support your child. For example, set interim goals together and reward your child for achieving them. This will help your child take small steps towards full bladder control.
Urotherapy for bedwetting
The first step on the road to nocturnal dryness is called urotherapy. During urotherapy, the child and parents are informed about how the kidneys and bladder work and what the young patient’s problem is. This increases the child's understanding and willingness to cooperate.

Your child should become aware of the processes in his or her body and learn to empty the bladder voluntarily. Simply changing incorrect drinking or toilet habits can often lead to significant improvement, and no further treatment is needed. It is also important to pay attention to your child's bowel movements. The elimination of constipation also often relieves the symptoms of enuresis.
The components of urotherapy include, for example:
- The child should drink majority of fluids during the first half of the day so that he/she is not as thirsty in the evening.
- The child should not have any sugary or caffeinated drinks in the evening.
- The child should always go to the toilet before going to bed.
You may want to introduce a reward system, such as stickers or pictures to colour in. This can motivate your child to get used to the changes. You can also try our colouring calendar (pdf, 6.37MB), stick-on calendar (pdf, 1.65MB) or bladder diary (pdf, 187KB) to support your little patient:
What medication is available for bedwetting?
If the doctor finds that your child is producing too much urine at night due to an ADH deficiency, a medicine with an active ingredient that is similar to the body’s own antidiuretic hormone and causes the same reaction in the body may help. Urine production is reduced at night, allowing your child to sleep through the night.
Medication proves to be very successful and is accompanied by side effects only in very rare cases. However, it is important that you seek detailed advice from your doctor and follow their instructionsexactly. Only they can determine the dosage and when to end the therapy.
Using the bedwetting alarm
Treatment with the bedwetting alarm is a successful treatment method if your child has difficulty waking up. Bedwetting alarms are available in two versions: Portable alarm pants (briefs) and alarm mat for the bed.

Both devices work on the same principle. Bedwetting alarms have a moisture sensor that sounds an alarm as soon as your child wets himself/herself while sleeping. This wakes up the child, who then has to go to the toilet to consciously empty the bladder fully. This undesirable experience of the alarm helps your child understand when his/her bladder is full and to wake up on his/her own.
In the first few weeks, it is essential that the alarm really wakes up your child. This is the only way to achieve the learning effect. This requires the understanding and acceptance of the whole family, as it is not uncommon for siblings to be woken by the alarm.
Ask your doctor to instruct you in the use of the bedwetting alarm. Make sure that your child also understands how it works and agrees to this treatment method. This treatment method has a great chance of success.
Tips for parents
There are a few things you can do to make everyday life as stress-free as possible for you and your child:
- Has your child been invited to spend the night at a friend's house? Talk openly with the parents; they often know these symptoms from their own experience.
- Keep bed sheets and pyjamas handy so that you can quickly get your bed fresh again if there is an accident.
- Protect the child's mattress with a waterproof cover.
- Disposable nappies for older children are available in shops. You can use them if you wish.
- Wash or shower your child in the morning to avoid unpleasant odours.
Always keep in mind: bedwetting is not unusual and the problem usually stops on its own at some point.
Specialist groups
For medical professionals
Which medicines are suitable for each type of bedwetting, how do they work, what are their dosages and side effects? Doctors can get all important information here.
Services
Free downloads on the topic of bedwetting
Here are some useful resources to help your child have fun and stay motivated during toilet training.
Hoppla – more than an online bladder diary
Hoppla is a website for young patients having problems with toilet training. It explains the topic in a child-appropriate manner. The integrated micturition diary can be used to document fluid intake, micturition and bowel movements in real time. The child's motivation is supported by a reward system.
With Hoppla, children learn a lot of interesting facts about their own bodies and about peeing. Hoppla also provides a drinking and toilet diary that children can playfully fill out themselves.
![[Translate to English:] Hoppla-Hase mit QR-Code zur Hilfe bei Einnässen bei Kindern.](/fileadmin/apogepha/werbung-ausserhalb-homepage/csm_hoppla-hase_60a61c9607.png)
Bedtime story
A calm and relaxed atmosphere helps children fall asleep. You can encourage this by reading a book or listening to a story together - so your child doesn't go to bed worrying about wetting himself/herself.
Here you can download the fairytale "The Steadfast Tin Soldier" by Hans Christian Andersen. Use the story as a nice evening ritual to create a relaxed atmosphere.
![[Translate to English:] Hilfe bei Einnässen bei Kindern: Zeichnung eines Jungen im Bett.](/fileadmin/apogepha/werbung-ausserhalb-homepage/csm_einnaessen-beim-kind-gutenachtgeschichten_f3efdc3c92.png)
Download the fairytale as an mp3 file from here:
The fairytale "The Steadfast Tin Soldier" has been made available by www.vorleser.net.
Downloads
Downloads
FAQs
Frequently asked questions and answers about bedwetting in children
Bedwetting can be caused by delayed bladder maturation, genetic factors, deep sleep, hormonal imbalances or stress. It is often caused by a combination of these factors.
Bedwetting is normal up to the age of about 5 years. By this age, many children develop full control over their bladder.
Regular visits to the toilet before going to bed, limiting fluid intake in the evening and having a quiet environment to fall asleep can prevent bedwetting. If problems persist, it may be a good idea to see a paediatrician.
In children, bedwetting may have psychological causes such as stress or anxiety, especially if it reoccurs suddenly after a long dry spell. A comprehensive examination can help determine the exact cause and treat it accordingly.
Get the cause of wetting clarified by your doctor. He/she can determine whether treatment is necessary and suggest a suitable therapy. Before using medication, a so-called urotherapy (normalisation of drinking and toilet behaviour) should take place.
Sources
- 1 Byrd et al., Pediatrics, 1996, 98:414-9 Kontinenzschulung im Kindes- und Jugendalter, Konsensusgruppe Kontinenzschulung im Kindes- und Jugendalter e.V., 2010, Pabst Science Publishers, Lengerich.
- 2 Bachmann, Claßen. Harn- und Stuhlinkontinenz bei Kindern und Jugendlichen, 2010, UNI-MED Verlag AG, Bremen.
- 3 „Wasser“. DGE, https://www.dge.de/wissenschaft/referenzwerte/wasser/. Zugegriffen 16. Juli 2024.


![[Translate to English:] Einnässen: Grafik eines Mädchens, das nachts traurig auf der Bettkante sitzt.](/fileadmin/_processed_/d/5/csm_Einnaessen-beim-Kind_Illustrationen-10_13b4d04d21.png)
![[Translate to English:] Kind wegen Einnässens bei der ärztlichen Diagnose.](/fileadmin/_processed_/2/0/csm_Einnaessen-beim-Kind_Illustrationen-4_99caefc908.png)

![[Translate to English:] Frau mit Wasserglas in der Küche: Viel trinken kann gegen eine Reizblase helfen.](/fileadmin/apogepha/mood-fotos-stock/AdobeStock_600884727.jpg)