Symptoms
Symptoms and types of urinary incontinence
The International Continence Society defines urinary incontinence as any involuntary urination – i.e., when it is not (always) possible for a person to control the time and place of urination.1 In this condition, urine is either passed constantly or in drops only in certain situations. Therefore, bladder weakness is not a disease in itself, but a symptom of an underlying disease of the urinary system.
As incontinence can have different causes and manifests itself in a variety of symptoms, it is in categorised into different types:
Urge incontinence is a bladder storage disorder. This causes the bladder muscle to contract even when the bladder is only slightly full, without the person being able to control it. The irrepressible (imperative) urge to urinate leads to involuntary urine loss.
Stress incontinence is triggered by a weakness of the pelvic floor muscles, the sphincter muscles and the connective tissue. Sneezing, laughing, coughing or running leads to involuntary loss of urine without previously having had the urge to urinate. Overweight women or men, women who have had multiple deliveries, older people or men after prostate surgery are especially affected by this type.
Mixed urinary incontinence is a combination of urge incontinence and stress incontinence. The symptoms of stress incontinence and urge incontinence are present to varying degrees. There is both involuntary urine loss during physical exertion and a strong urge to urinate.
Neurogenic bladder emptying disorders are the result of damage to the nervous system due to illness, accident (especially when there is traumatic damage to the spinal cord) or congenital malformations. Damage to the nervous system disturbs the interaction of all nerves and organs involved in urine storage and emptying. Those affected no longer have any control over the emptying of the bladder and usually do not feel any urge to urinate.
Experts refer to overflow incontinence as “incontinence with chronic urinary retention” as well. It is typically characterised by urine dribbling without any noticeable urge to urinate. This can be caused by so-called drainage disorders (problems emptying the bladder, for example in the case of benign prostate enlargement or urethral injury). Diminished function of the bladder muscle is also a possibility (for example in some neurological diseases). During a visit to the toilet, the affected person cannot fully empty the bladder even when it is full and residual urine remains in the bladder.
This is characterised by involuntary loss of urine through channels other than the urethra. It can be congenital or caused by injury (e.g., malocclusions of the ureter or bladder fistula). The storage function and closure mechanism of the bladder are not affected.
Incidence
How often does incontinence occur in women and men?
Urinary incontinence is a widespread disorder that occurs in all cultures. Numerous people are affected: In Germany alone, an estimated 6 million men and women suffer from bladder weakness.2 The number of affected people increases with age.
In our society, urinary incontinence still carries a strong stigma. The ability to control the bladder is a milestone in a child's development. When people no longer have complete control over the bladder, they often feel ashamed and give up familiar activities such as going to the theatre, playing sports or even travelling. Experts therefore also suspect a highnumber of unreported cases.
Urinary incontinence in women
On average, women suffer 2 to 4 times more frequently from the symptoms of bladder weakness than men.3 This is primarily due to the anatomy and physiology of the pelvis. With increasing age, however, the incidence of the disease in both sexes becomes similar.
Due to the ability to become pregnant and give birth, the female pelvis is more flexible than the male pelvis and the pelvic floor is under greater stress. In addition to passages for the ureter and rectum, the female pelvic floor also has an additional passage for the vagina, which weakens the strength of this muscular pelvic closure. However, urinary incontinence often also occurs after menopause due to oestrogen deficiency.
![[Translate to English:] Infografik veranschaulicht die Häufigkeit von Inkontinenz bei Frauen und Männern in Deutschland: Betroffen sind 13 % aller Frauen, 5 % aller Männer; bei den über 60-Jährigen 19 % der Frauen und 10 % der Männer; insgesamt sind etwa 30 % der Patienten über 80 Jahre alt.](/fileadmin/_processed_/b/c/csm_img-inkontinenz-v2_b425fd4508.png)
While young women often suffer from stress incontinence alone, the proportion of urge incontinence and mixed incontinence increases with age.
![[Translate to English:] Grafik zeigt die Häufigkeit von verschiedenen Formen der Blasenschwäche bei Frauen: 50 % Belastungsinkontinenz, 33 % Mischinkontinenz und 17 % Dranginkontinenz.](/fileadmin/_processed_/7/8/csm_pie-chart-inkontinenzarten_d4a5f9377f.png)
Urinary incontinence in men
Men, especially young men, suffer much less frequently from incontinence than women.3 This is mainly because the male pelvic floor is not exposed to pressure from pregnancy and childbirth.
In general, men of all ages are predominantly affected by overactive bladder or urge incontinence. In younger men, incontinence usually only occurs as a result of a neurological disease or bladder and urethral narrowing, urinary stones and bladder infections. Rare congenital male urinary incontinence due to anatomical defects is usually corrected surgically in childhood.
In older men, difficulty in emptying the bladder and residual urine indicate a possible benign enlargement of the prostate.
Urinary incontinence in old age
Along with dementia and faecal incontinence, weak bladder is one of the most common age-related conditions in people over 65.
In retirement and nursing homes, the number of patients suffering from bladder weakness is significantly higher than average. Up to 80 percent of the women and men there are affected by this due to age.2 Urge incontinence is most common in people who need care.
Reasons for this include low mobility and the resulting difficulty in reaching the toilet in time. In addition, existing urinary incontinence is often the main reason for admission to a nursing home.
Trigger
Causes and risk factors of incontinence
There are a number of factors that can stimulate or even cause urinary incontinence. Some of these can be controlled by the affected individual's will, while others are beyond their control.
Numerous studies have shown a clear link between increasing age and urinary incontinence. Of all the risk factors, a patient's age has the greatest influence on the incidence of bladder weakness. This is primarily due to age-related changes in the urinary system.
Up to the age of about 60, women are more frequently affected by bladder weakness than men. This is mainly due to the anatomical differences between the two sexes.
Studies have shown that there is a clear link between incontinence and pre-existing conditions such as depression, stroke and diabetes mellitus. Some diseases are also indirect risk factors because the medicines used to treat them affect the way the urinary system works.
Physical activity, especially a well-trained and relaxed pelvic floor, reduces the risk of incontinence. If incontinence exists, physical activity helps to alleviate the symptoms. Strengthening the pelvic floor is particularly important after surgery, pregnancy and delivery. However, only continuous training can ensure the long-term success of the treatment. Pelvic floor training can also be done using special vaginal cones.
An unhealthy lifestyle can contribute to the development of urinary incontinence. Excess weight leads to a chronic increase in pressure on the pelvic floor, which cannot compensate for this pressure in the long term. For smokers, smoker's cough in particular can put extra strain on the pelvic floor. Smoking is also very likely to be a risk factor in itself. Physical and mental stress can also be risk factors for bladder weakness.
Pregnancy and natural delivery put a lot of strain on the lesser pelvis and especially the pelvic floor.
Surgical procedures or radiotherapy in the lesser pelvis increase the risk of urinary incontinence. In particular, surgical removal of the uterus in women or the prostate in men is associated with an increased risk.
There is evidence that incontinence runs in families. For example, children have a higher risk of bedwetting if there are other people in the family who used to wet the bed.
Diagnosis
This is how a doctor diagnoses bladder weakness
The basic diagnosis can be carried out by the GP as well as the urologist or gynaecologist. This includes the following measures:
The general medical history is the starting point for any diagnosis. Ideally, it begins with an open discussion between patient and doctor. The main purpose is to break down the taboos surrounding urinary incontinence and to build a relationship of trust between patient and doctor. During the discussion, the doctor asks questions about the patient’s medical history and existing concomitant illnesses and treatments. However, the patient's lifestyle also plays a decisive role in drawing attention to possible risk factors. For women, the menstrual cycle, menopause or the onset of menopause, pregnancies and deliveries are also discussed.
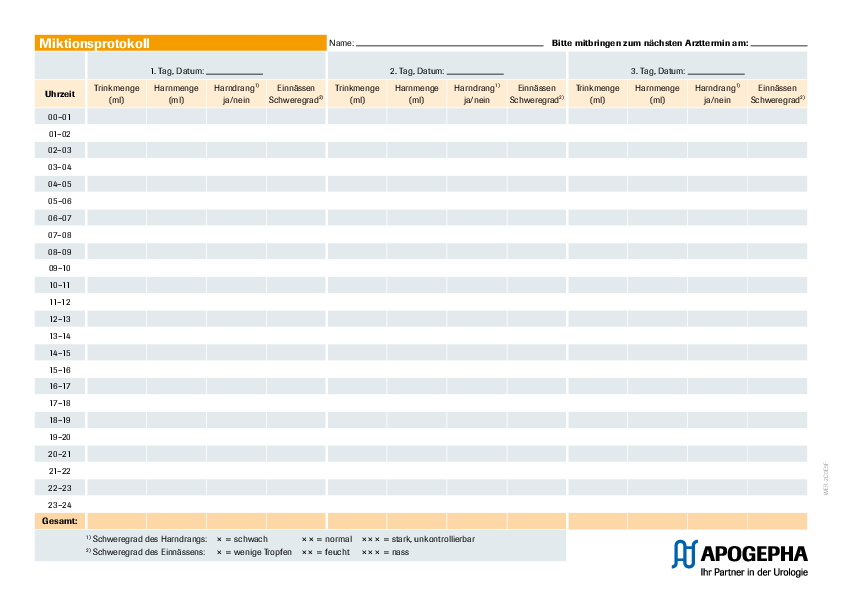
The micturition history is used to analyse any storage or closure problems of the urinary bladder. In particular, the doctor records the patient's drinking and micturition habits. These include the daily fluid intake in relation to the number of visits to the toilet during the day and at night, as well as any habits such as holding back urine when the bladder is full or squeezing the stomach when urinating.
Recording toilet visits and fluid intake is a key component of basic diagnosis. The severity and type of urinary incontinence can be assessed with the help of the drinking and micturition diary. The patient records the number of visits to the toilet, the amount of urine and any incontinence episodes and the fluid intake in detail over a period of 2 to 3 days. You can easily download a pre-designed template from here.
This way, you become aware of the bodily functions that are otherwise carried out unconsciously and they can be consciously observed. Complete documentation requires a high degree of cooperation on the part of the patient. It is advisable to do this over a weekend in a stress-free and familiar environment.
An incontinence questionnaire is used to determine the type and severity of incontinence. The 16 questions are rated with points depending on the answer. The total sum then results from the addition of all points and provides information about the type of incontinence, its severity, and the recommended treatment.
During the examination, the doctor looks for external abnormalities such as inflammation, scarring and changes to the mucous membrane. The examination comprises the following steps: external examination of the abdomen, examination of the external reproductive organs, rectal examination, vaginal examination and cough test. The cough test is used to check whether the patient loses urine under stress when the bladder is filled with a medium amount of urine.
Urinalysis is carried out with freshly passed midstream urine. Blood admixtures, protein and bacteria in the urine are detected and the pH value is determined by means of test strips.
During the sonographic examination, the upper and lower urinary tract (especially the kidneys and the ureter) are checked to rule out scarring, inflammation or urinary transport disorders as causes for bladder weakness. In addition, residual urine and the thickness of the bladder wall can be measured. Ideally, sonography should be performed both when the bladder is full and when it is empty.
In most cases, the individual results can be used to determine the type of urinary incontinence the patient has. This and an open approach to the condition lays the foundation for successful treatment
Further diagnostic measures are only necessary if the basic diagnosis indicates the possibility of complicated urinary incontinence or if none of the therapeutic measures based on the basic diagnosis have been successful. They are carried out by a specialist (urologist) and include the following examinations:
During cystoscopy, the bladder and urethra are examined with an endoscope. Anaesthesia is not usually required for this procedure. The examination is usually performed as a so-called video urethrocystoscopy. Here, the image taken with a camera mounted on the endoscope is transmitted to a screen. This examination can be used to examine the bladder sphincter and to check the bladder for foreign bodies, tumours and inflammation.
X-ray examinations of the bladder and urethra are used to see so-called fistulas, dropping of the bladder, urethral narrowing, prostate enlargement, incomplete emptying of the bladder and bulges of the bladder. A contrast medium can be used for better detection.
If there are indications that the incontinence may be caused by disorders of the nervous system, additional neurological diagnosis will be needed.
Urodynamics is used for checking the functioning of the urinary bladder. During filling, the bladder pressure is measured when the bladder is relaxed and during exertion (coughing) to detect involuntary contractions of the bladder muscle. Whether and how much urine is lost when the bladder fills as well as the bladder volume are also recorded.
Uroflowmetry is a simple, non-invasive test that measures urine flow as the bladder empties. Possible problems with emptying the bladder are identified.
A blood test is performed to check the blood sugar level, rule out infections and check for other urinary bladder conditions.
Important:
Patients often only consult a doctor when their suffering becomes unbearable. The reasons for this are the fear of unpleasant examinations and the reluctance to discuss symptoms and complaints with a doctor.
Moreover, the widespread belief that urinary incontinence is not a real medical problem can also be a barrier to seeking medical help. The fact is, however, that the majority of incontinence diseases can be adequately diagnosed only through thorough anamnesis and other simple examinations.
Treatment
Treatment of urinary incontinence
This condition can often be positively influenced by behavioural changes. Medication with so-called urological spasmolytics can also be used. These calm the bladder muscles and increase the capacity of the bladder.
Conservative measures to strengthen the pelvic floor muscles, such as pelvic floor exercises, pelvic floor training with vaginal cones, electrostimulation or vibration therapy, are at the centre of the treatment. Medication is possible with oestrogens (especially for women experiencing menopause) or with medicines that stimulate the closure mechanism of the urinary bladder. In severe cases, surgical methods are indicated, such as inserting a band or loop to support the structure of the urinary bladder.
In this type of incontinence, both the urge and stress components must be treated according to the therapeutic options listed above.
The aim of the therapy is normalisation of the internal bladder pressure using urological spasmolytics, mostly in combination with catheterisation. As an alternative to this medication, the uncontrolled contractions of the bladder muscle can also be prevented by injecting botulinum toxin type A. If these methods are not successful, a surgery may be an option, such as urinary diversion through the abdominal wall, bladder enlargement (augmentation) or neuromodulation.
In the event of overflow incontinence due to narrowing of the bladder outlet, the narrowing must be eliminated. This is usually performed by means of a surgical intervention (e.g., in the case of benign prostate enlargement, with prostate resection). If overflow incontinence is due to a weak bladder muscle, it is necessary to drain the urine via a catheter. Alternatively or in addition, the bladder muscle can be activated with medication or electrostimulation.
The aim of the therapy is the surgical removal or correction of a malformation or injury.
Products for overactive bladder
So-called urological spasmolytics can be used as medication for overactive bladder/urge incontinence and neurogenic detrusor hyperactivity. These calm the bladder muscles and increase the capacity of the bladder. Urological spasmolytics are available on prescription only. It is therefore essential to consult a doctor before starting this treatment.
To reduce the number of visits to the toilet, regain continence and improve overall quality of life, patients can also benefit from comprehensive bladder and pelvic floor training in line with the guidelines.
Prevention
Preventive measures against bladder weakness
- Avoid being overweight (obesity) by eating a healthy diet and engaging in physical activity.
- However, avoid sports that can damage the pelvic muscles through constant or periodic pressure, such as trampolining.
- With smokers, the constant irritable cough in smokers' bronchitis can cause or worsen stress incontinence. Quitting is therefore the best precaution.
Where can I find help?
At the German Continence Society (DKG), there are numerous self-help groups where you can find advice and understanding for your complaints. Here you can also find out which doctors offer consultations on urinary incontinence and where you can find pelvic floor and continence centres in your region.
Specialist groups
Information for specialist medical groups
To access detailed product information on the treatment of urinary incontinence after using the specialist group login, click here:
Downloads
Free service material for download
You can download free service material on urinary incontinence from here:
FAQ
Questions and answers about urinary incontinence
Going to the toilet up to 8 times a day is normal unless urination is accompanied by a strong, irrepressible urge to urinate. In that case, you should see your doctor. He/she can prescribe the appropriate treatment for you.
Bladder weakness occurs more frequently in old age. It is important to find out when it occurs. Depending on the type, your doctor can find a suitable treatment option - from pelvic floor exercises and medication to surgery.
Medication for urge incontinence is a permanent therapy. In most cases, the symptoms reoccur when medication is discontinued. If you tolerate the medication very well, there is no need to stop it. If you are unsure, consult your doctor.
Unfortunately, urinary incontinence often occurs after prostate surgery. It is important to strengthen the pelvic floor muscles again, for example through pelvic floor training. Doctors can treat a strong, irrepressible urge to urinate with medication (bladder spasmolytics).
Signs of incontinence include uncontrollable urination, sudden urge to urinate, loss of urine on exertion or coughing and frequent urination at night. You should consult a doctor if these symptoms occur regularly.
Sources
- 1 “Urinary Incontinence”. International Continence Society, https://www.ics.org/glossary/sign/urinaryincontinence. Accessed on 18 July 2024.
- 2 "Bladder weakness (urinary incontinence)". Federal Ministry of Health (BMG), https://gesund.bund.de/inkontinenz-und-blasenschwaeche. Accessed on 18 July 2024.
- 3 “Urinary incontinence”. Robert Koch Institute, Federal Statistical Office, https://edoc.rki.de/bitstream/handle/176904/3191/26Herxag1MT4M_31.pdf?sequence=1&isAllowed=y. Accessed on 18 July 2024.


![[Translate to English:] Älteres Paar in einem Boot: Harninkontinenz tritt im Alter häufiger auf.](/fileadmin/_processed_/b/1/csm_csm_blasenschwaeche-paar-im-paddelboot_cbc338656b_d0e216bfca.png)
![[Translate to English:] Älteres Paar beim Tanzen: Das Alter ist ein Risikofaktor für Harninkontinenz.](/fileadmin/_processed_/2/4/csm_csm_paar-tanzt-am-meer_96e602ff43_9e573151f9.png)
![[Translate to English:] Patient im Gespräch mit dem Urologen wegen seiner Harninkontinenz.](/fileadmin/_processed_/f/b/csm_AdobeStock_336336436_7d74f987e1.jpg)
![[Translate to English:] Frau ist ausgelassen am Strand, da sie ihre Blasenschwäche dank Therapie im Griff hat.](/fileadmin/_processed_/4/9/csm_csm_harninkontinenz-glueckliche-frau_96d7a65a3c_d08329afd2.jpg)


![[Translate to English:] Frau mit Wasserglas in der Küche: Viel trinken kann gegen eine Reizblase helfen.](/fileadmin/apogepha/mood-fotos-stock/AdobeStock_600884727.jpg)
