Bladder cancer
This can be benign or malignant. Malignant tumours originating in the bladder are called bladder carcinomas.

How cancer develops is still largely unexplained.
It develops in the cells of our body. Healthy cells grow, divide and multiply in order to maintain the health and functionality of the body. However, they can get out of control. They start dividing uncontrollably. These excess cells form a tumour.
Symptoms of bladder cancer
The cause of the development of malignant tumours has not yet been definitively determined. However, there are a number of factors that increase the risk of a bladder tumour. Smoking is a major risk factor. Contact with certain chemical substances (especially aromatic amines) can increase the risk of developing a bladder tumour. People who have worked with these chemicals and have developed a bladder tumour can have this cancer recognised as an occupational illness. This can include activities in the chemical and pharmaceutical industry, rubber industry, paint applications in the painting trade, textile industry, leather processing, printing houses, refineries, coking plants, gas works or chimney sweeping. Although occupational safety measures have greatly reduced the risk today, occupational transitional cell carcinomas can still occur because the development time (latency period of up to 40 years) for this tumour is very long.
Other risk factors include chronic cystitis, frequent use of painkillers containing phenacetine or an infectious disease that lasts for years.
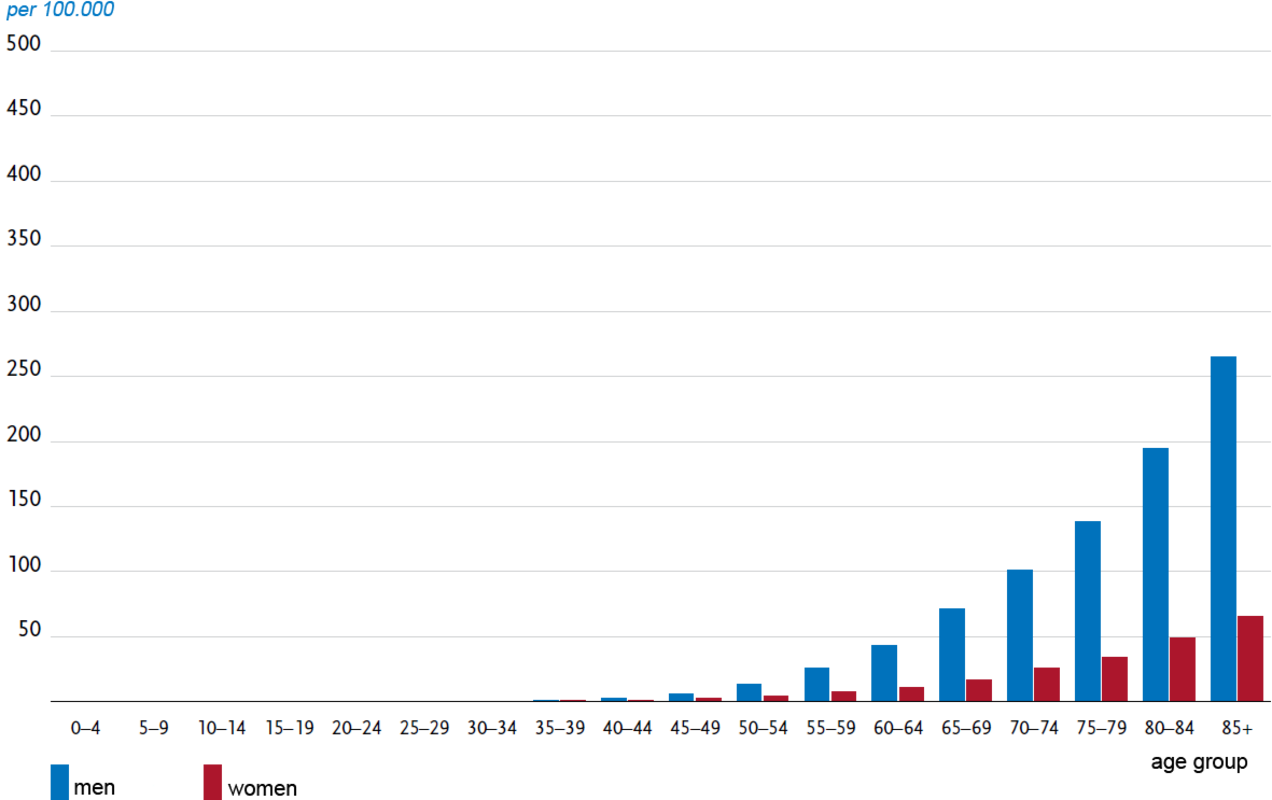
Approximately 29,500 new cases of bladder tumours were predicted for the year 2018 in Germany. Men are affected two to three times more frequently than women. The average age of the onset of the disease is 74 for men and 76 for women (see diagram).
Symptoms – How can I recognise bladder cancer?
Often, there are no early symptoms of bladder cancer. Bladder cancer gives rise to hardly any complaints in the early stages. Bleeding of the tumour (macrohaematuria) is often painless. This symptom occurs in about 80% of patients with bladder cancer. The urine is reddish to brown. Furthermore, frequent urination (pollakiuria) or urge to urinate without any urine being passed or unspecific subjective complaints can be an indication of bladder cancer. In the advanced stages, pain may occur in the lateral body trunk, palpable tumour in the abdominal area, enlargement of lymph nodes, lymph or vein congestion or bone pain.
The listed symptoms may indicate a malignant disease of the bladder, but there are other possible causes, which are completely harmless. In any case, this should be clarified by a urologist, because bladder cancer in its early stages can be treated and is permanently curable.
Bladder cancer diagnostics
Bladder cancer diagnostics is carried out for patients with the following symptoms:
- Macrohaematuria
- Chronic macrohaematuria
- Persistent dysuria (unpleasant, difficult or painful emptying of the bladder) or symptoms of urge to urinate.
The following examinations can be conducted for diagnosis:
The starting point in most cases is a detailed conversation, the anamnesis. The urologist obtains an idea of the current symptoms, previous illnesses and possible risk factors. A thorough physical palpation can also provide further information. Subsequently, various physical and analytical examinations are carried out so that a clear diagnosis can be made.
Testing of urine and blood samples
At first, questions such as the ones below must be answered: “Are traces of blood be found in the urine?” or “Are the blood values okay?”. Urine and blood samples are thoroughly tested in the laboratory. The urinary cytology method in particular (examination of urine for pathological cell components, particularly cancer cells) can diagnose diseases of the urinary bladder, urinary tract and renal calyx system at an early stage.
Urography
If blood has been detected in the urine, then a urography of the kidneys, ureter and bladder is performed. This method gives the urologist an overview of the entire urinary tract.
Biopsy
In a biopsy, tissue samples are removed from the body for histological examination under the microscope by a pathologist. Removal can take place directly during cystoscopy using the endoscope. This examination is often the only reliable method to exclude or diagnose bladder cancer without any doubt.
Ultrasound
An ultrasound of the lower abdominal region, the kidneys and the bladder is performed to detect any changes in the internal organs. Abnormalities indirectly indicate a tumour.
Cystoscopy
Cystoscopy is performed to examine the mucous membrane of the bladder. A thin, soft and flexible tube (endoscope) is inserted through the urethra into the bladder. The tube is fitted with a camera and a light source. As a result, the size, extent, location of a tumour or even several existing tumours can be detected. Cystoscopy is necessary to confirm the final diagnosis and to plan surgical therapy. It is usually a low-complication and largely painless examination.
Tumour marker
Some tumour markers (e.g., NMP-22) are also used for diagnosis. However, their use is currently controversial in research and they have not yet been widely used.
Further investigations in the case of invasive tumours
T-stages and grading are important prognostic factors that determine the subsequent therapeutic measures. If an invasive bladder carcinoma is present, further investigations are necessary to detect possible metastases. Diagnostic methods include computer tomography (CT), magnetic resonance imaging (MRI) and skeletal scintigraphy.
Treatment of bladder cancer
If a bladder carcinoma is detected and treated in time, there is a good chance of complete recovery. The respective treatment and its success are directly related to the classification of the tumour.
An important point that you can influence on your own: if you are a smoker, consider to quit or reduce smoking! Smoking is the main risk factor for the development of bladder carcinoma.
Basically, during therapy, a distinction is made between non-invasive and invasive bladder carcinomas because the procedures in the respective therapy differ considerably. The therapy for non-invasive bladder carcinoma is presented here.
Therapy for non muscle invaisve bladder carcinoma
Non-invasive carcinomas account for about 80% of diagnosed bladder cancers. With a proper treatment these have a good chance of recovery as they usually have a low malignant potential.
If this tumour is unilocular (occurring at one place), it is removed through transurethral resection of the bladder (Transurethral resection-B) followed by early instillation. Here, medication is flushed directly into the bladder using a catheter. Multilocular bladder Tumors (occuring in several places), tumours with high malignant potential or a CIS (carcinoma in situ) must be treated further. It is a known fact that these tumours often relapse (recurrence of the tumour) and are progressive. Depending on the classification, adjuvant (concomitant) intravesical instillation therapy with chemotherapeutics or immunotherapeutics is recommended after surgical removal of the tumour tissue.
This instillation therapy begins with early instillation, which is usually performed within two to a maximum of 24 hours after removal of the tumour. This can prevent the nesting of loosened tumour cells and thus reduce the risk of recurrence.
Only a cytostatic drug is used for early instillation. Depending on the course of surgery and the classification of tumours, the instillation therapy is continued immediately or after healing of the surgical wound either with chemotherapeutics (substances that damage or kill tumour cells in the organism) or immunotherapeutics (activation of the immune system through pharmaceutically active substances).
This chemotherapy is the so-called intravesical (into the bladder) chemotherapy. The cytostatic drug (substance that inhibits cell growth or cell division) is instilled (flushed) directly into the bladder using a catheter (tube). The most widely used drug in Germany is mitomycin (MMC). It can inhibit the growth of cancer cells and kill them.
The most important immunotherapeutic agent is BCG (Bacillus Calmette-Guerin). It is an attenuated bacterium. This means that the bacteria can no longer cause infection, but they can cause an immune response. The BCG causes a defence reaction that is concentrated on the bladder. As a result, residual tumour cells can be combated and an immune response to the tumour cells can be generated.
The method used is the same for both substances:
The substance is dissolved in a saline solution and introduced into the bladder using a disposable catheter. It remains there for one to two hours and is then excreted normally into the toilet.
For detailed information on these treatment methods, please refer to the Mitomycin Patient Guide and Mitomycin Patient Alert Card.
Precautions for bladder cancer
There is no screening for early detection of bladder cancer, which is recommended for the general population currently.
The best prevention is a smoke-free life as well as healthy eating and living habits.



