Prostate cancer -
Check-ups are essential
Prostate cancer
The earlier prostate cancer is diagnosed, the better are the chances of treatment and even recovery. If the cancer is still in its early stages, i.e., limited to the prostate for instance, then the chances of recovery are relatively good.
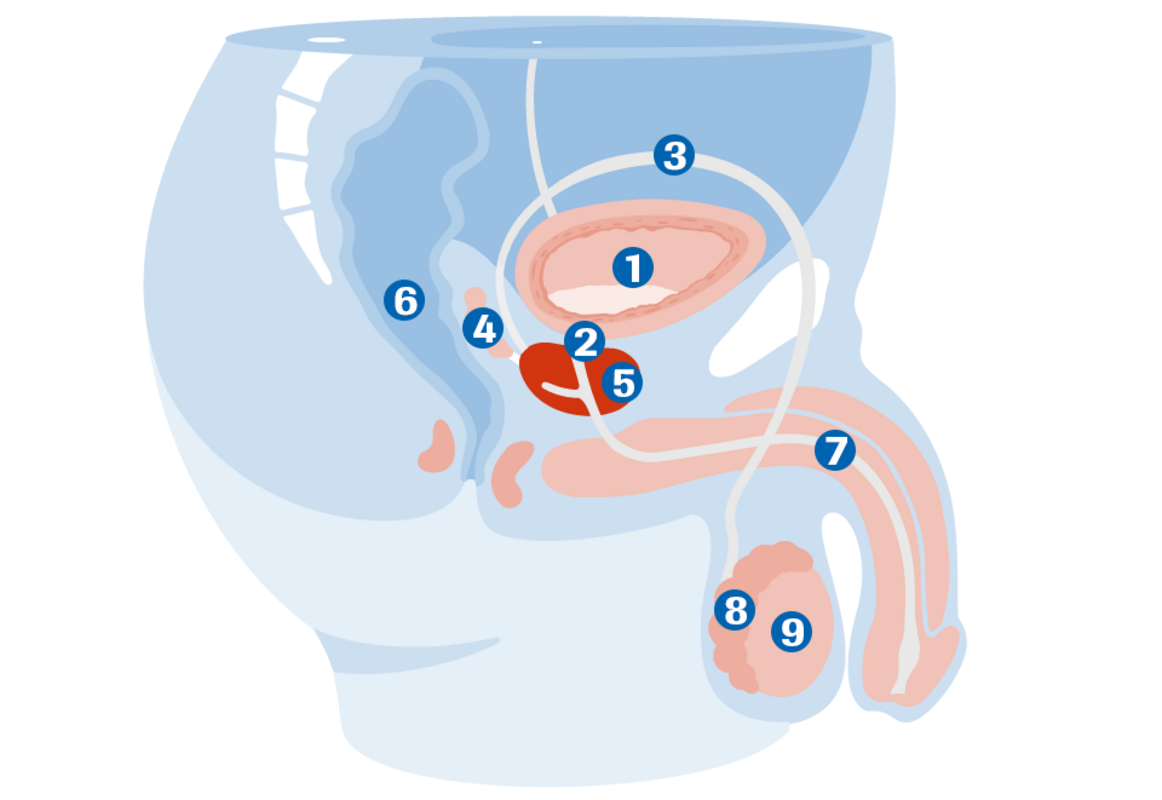
The prostate
The prostate is located below the bladder and surrounds the urethra in the form of a ring. In common parlance, it is also known as the “prostate gland” and is chestnut-sized when in a healthy condition.
In the course of a man's life, the prostate grows steadily from the age of 40. This is a normal and physiological process called benign prostate enlargement (BPH= Benign Prostatic Hyperplasia). This benign prostate enlargement is completely different from prostate cancer in its development and progression.
(1) Bladder
(2) Bladder neck
(3) Spermatic duct
(4) Seminal vesicles
(5) Prostate
(6) Rectum
(7) Urethra
(8) Epididymis
(9) Testicle
Causes, development and incidence
The causes of prostate cancer are not fully understood. The following factors probably contribute to its development:
- Hormone status
- Hereditary disposition
- Diet
- Age
- Unhealthy lifestyle
Prostate cancer is the most common type of cancer in men in the western industrialised countries. In Germany, almost 60,000 men contracted prostate cancer in 2014. Prostate cancer is the third-most common cause of cancer-related death. About 13,700 men die from this disease every year.
The incidence of this disease increases with age. The average age at the time of diagnosis is 72 years. In recent years, the mortality rate has decreased significantly because prostate cancer can now be diagnosed earlier and earlier. In the early stages, prostate cancer can often be treated successfully. But even at an advanced stage, prostate cancer can often be controlled and successfully treated over many years.
What are the symptoms?
At the very initial stages of the disease, hardly any symptoms can be detected. Prostate cancer often develops in the outer regions of the gland and narrows the urethra only after the cancer is already quite large. In prostate cancer, symptoms (weak urine stream, urinary stuttering, post-micturition dribbling, frequent urination) as well as unspecific symptoms such as rheumatic pains, reduced performance or blood in the urine or semen can indicate a late stage of the prostate disease. Sciatica and bone pain can be caused by secondary tumours (metastases). Acute impotence may also indicate the presence of prostate cancer.
This is why annual urological check-ups are so important!
Diagnostics of prostate cancer
The earlier prostate cancer is diagnosed, the better are the chances of treatment and even recovery. If the cancer is still in its early stages, i.e., limited to the prostate for instance, then the chances of recovery are relatively good.
Diagnostic examinations: Digital Rectal Examination (DRE): The urologist feels his finger through the rectum and can feel benign enlargements, suspicious lumps and hardenings.
Transrectal ultrasound and determination of the PSA value are useful supplements. Multiple PSA values should always be taken over a period of time. The ratio of free PSA to total PSA provides a further indication of the presence of prostate cancer.
In general, the indicative values are:
- Normal range: 0 - 4 ng/ml
- Grey range: > 4 - 10 ng/ml
- Range in the case of suspected cancer > 10 ng/ml
Further investigations
A biopsy provides clarity. It involves the targeted removal of prostate tissue through the rectum using a hollow needle. The tissue is removed under local anaesthesia. The microscopic examination of the tissue samples taken reveals within a few days whether prostate cancer is present and how the tumour can be classified. Classification is important because therapy depends on the classification of the tumour.
DRE
Digital (with the finger) Rectal (through the anus) Examination. This method (palpation) is used to examine the prostate.
Biopsy
Removal of prostate tissue through the rectum using a hollow needle. A biopsy can clarify whether tumours are malignant or benign.
PSA
Prostate-Specific Antigen. This protein is produced by the prostate cells. An increase in its value (> 4 ng/ml) may indicate prostate cancer. However, several examinations are necessary for this.
Therapy for prostate cancer
Treatment depends on the result of the microscopic examination (biopsy result) and the spread of the tumour or metastases and must be adapted to the individual situation of the patient.
The main therapy options are:
- Watchful waiting/Active surveillance
- Surgery
- Radiation
- Anti-hormonal therapy
- Chemotherapy
These therapy options are also used in combination. When tumours are limited to the prostate, radical prostatectomy is the method of choice for permanent cure.
If prostate cancer is in an advanced stage, i.e., the tumour is widespread locally or there are metastases, the tumour is no longer curable. However, further adjuvant therapy options are available. Radical prostatectomy is useful until stage T1-3 N1 M0. Adjuvant hormone therapy, which is effective throughout the body, is used in more advanced stages (T1-4 N1 M1) and metastasis. Chemotherapy is offered as an option if prostate cancer no longer responds adequately to hormone therapy. A castration-resistant tumour cannot be cured but it is possible to continue to control the progression of the disease.
DRE
Digital (with the finger) Rectal (through the anus) Examination. This method (palpation) is used to examine the prostate.
Biopsy
Removal of prostate tissue through the rectum using a hollow needle. A biopsy can clarify whether tumours are malignant or benign.
PSA
Prostate-Specific Antigen. This protein is produced by the prostate cells. An increase in its value (> 4 ng/ml) may indicate prostate cancer. However, several examinations are necessary for this.
Happy life - despite prostate cancer.
Last year, at my wife's urging, I went for a screening test. Actually I didn't want to go, somehow it made me uncomfortable. But today I'm glad I listened to her. At that time I had an elevated PSA level.

What is hormone therapy?
The male sex hormone testosterone (androgen) is required for the healthy functioning of a prostate. However, it also promotes the growth of carcinoma. This is also called the 'hormone dependence' of prostate cancer. This hormone dependence is used in the therapy for this cancer.
Testosterone production in the testicles is prevented through surgical removal of the testicles or by medication that blocks the effect of the hormone. This often stops the growth of prostate cancer for years.
Antiandrogenic therapy with (luteinising hormone releasing hormone) agonists (e.g., buserelin, leuprorelin) and newer antihormonal substances (abiraterone, enzalutamide, apalutamide) is available today.
LH-RH agonists are administered into the skin (subcutaneous) as time-release drugs that continuously release the active ingredient. As a rule, this happens every 3-6 months. Side effects, such as hot flushes, a decrease in sexual drive and impotence are consequences of testosterone withdrawal. Since testosterone production increases at the beginning of therapy with an LH-RH agonist, an additional anti-androgen (e.g., bicalutamide) is given.
An LH-RH antagonist (degarelix) achieves a similar effect. It directly blocks the receptors on the pituitary gland and thus inhibits the formation of the hormones necessary for prostate cell growth.
Newer substances also lower testosterone, either by inhibiting the corresponding enzymes or at the corresponding receptors of the prostate cells. These newer active ingredients are always administered in combination with LH-RH agonists or antagonists.
Prostate carcinomas become hormone-refractory over time. This means that they no longer react to antihormonal therapy and the disease progresses.
Chemotherapy with cell growth inhibiting drugs (cytostatic drugs) is not suitable for slow-growing prostate cancer and is only used palliatively in the final stage. To relieve pain, bone metastases are irradiated and treated with bisphosphonates. Radiation can also be used as a therapeutic measure if, for example, surgery is not possible.
What can I do?
All therapies more or less affect your sexual interest and potency. This can lead to problems and misunderstandings with partners. Talking openly with your partner can help you successfully handle your illness and perhaps open new ways to achieve a fulfilling partnership.
An intact immune system is also important. Do yourself some good! Make sure you eat a balanced, healthy diet. Exercising in fresh air can also have a positive effect on your general well-being. Light and regular endurance sports are ideal.
Make appointments for check-ups so that any progression of the tumour can be detected and counteracted quickly.
If hormone therapy is used, a bone examination should be carried out every 1-3 years owing to the increased risk of osteoporosis.
Check up of prostate cancer
Have annual urological check-ups done.
All legally insured men aged 45 and above are entitled to a preventive urological check-up every year (in Germany).
Preventive check-ups help in detecting existing illnesses as early as possible. Half of all cancers could be prevented or diagnosed early and thus permanently cured, if risk factors (e.g., smoking and poor diet) are avoided and early detection screenings are regularly performed.
